Are you or a loved one struggling with substance abuse and seeking treatment covered by Aetna insurance? Understanding your options for drug rehabilitation can be overwhelming, but you’re not alone. In 2021, over 40 million Americans had substance use disorders, yet only 4 million received treatment. Aetna, a leading health insurance provider, offers coverage for various addiction treatment programs, including:
This guide will help you navigate Aetna’s drug rehab coverage, ensuring you can access the care you need to begin your journey to recovery.
Call Evoke Wellness at Miramar today (833) 819-6066or reach out online.
Understanding Aetna Insurance Coverage for Addiction Treatment
Substance Use Treatment Programs
- Aetna provides coverage for a range of evidence-based substance use treatment programs, including outpatient services, intensive outpatient programs, and inpatient rehab.
- Their plans cover medically necessary services for addiction treatment, such as medical detox, individual and group therapy, and medication-assisted treatment.
Dual Diagnosis Treatment
For those struggling with co-occurring mental health and substance use disorders, Aetna plans offer coverage for integrated dual diagnosis treatment programs. This approach simultaneously addresses both conditions for better treatment outcomes.
Residential and Extended Care
Aetna insurance plans may cover the costs of residential rehab programs, which provide 24/7 monitored care and support in a therapeutic environment. Extended residential care is also an option for those requiring a longer treatment duration.
Therapy and Counseling
Depending on the plan, Aetna may cover individual, group, and specialized therapy approaches like acceptance and commitment therapy (ACT). These evidence-based therapies are essential for addressing the root causes of addiction and developing coping strategies.
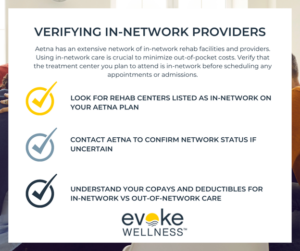
Verifying Coverage
To maximize your Aetna benefits, it’s crucial to work closely with the treatment center’s admissions team. They can help verify your specific coverage details and ensure you receive the appropriate level of care under your plan.
By understanding your Aetna insurance coverage for addiction treatment, you can make informed decisions about your recovery journey and access the comprehensive care you need.
Types of Treatment Covered by Aetna for Substance Abuse
Aetna recognizes addiction as a chronic disease, and provides comprehensive coverage for various evidence-based substance abuse treatment programs. Their website states that they cover treatments backed by clinical research and medical societies.
Inpatient & Residential Programs
- Medical detox to safely manage withdrawal symptoms
- Inpatient or residential treatment for 24/7 therapeutic care
- Dual diagnosis treatment for co-occurring mental health disorders
Aetna plans typically cover 30, 60 or 90 days of inpatient rehab, depending on the policy and medical necessity. Extended residential care may be approved for complex cases.
Outpatient Treatment
- Intensive outpatient programs (IOPs) with 9-20 hours of therapy per week
- Standard outpatient with fewer weekly sessions
- Medication-assisted treatment using FDA-approved drugs
Outpatient programs allow patients to live at home while receiving counseling, group therapy, and other services.
Therapy & Counseling
- Individual, group, and family therapy
- Evidence-based therapies like cognitive behavioral therapy (CBT)
- Mental health services for conditions like depression or trauma
- Aftercare programs to prevent relapse after completing rehab
According to SAMHSA, 19.3 million Americans aged 18 or older battled a substance use disorder in 2020. With comprehensive coverage from Aetna, those struggling can access high-quality, personalized care to achieve long-term sobriety.
Checking Your Aetna Plan Benefits for Rehab
Reviewing Your Coverage
Before beginning substance abuse treatment, carefully review your Aetna health insurance plan details. Understand what is covered for rehab services like detox, residential care, therapy and medications. Many plans cover at least some portion of evidence-based treatment programs.
Pre-Certification Requirements
Some Aetna plans require pre-certification or pre-authorization for certain levels of care like inpatient rehab. Not obtaining pre-approval could result in higher out-of-pocket costs or claims being denied.
Reach out to Aetna’s substance abuse treatment team to understand requirements for your specific plan and diagnosis. With pre-certification, Aetna can assist in locating appropriate in-network treatment options covered under your benefits.
Getting Aetna to Pay for Your Rehab Stay
Understanding Your Coverage
Your Aetna health insurance plan likely covers some level of substance abuse treatment. The key is understanding what is covered, any limitations or requirements, and navigating the approval process. Reach out to an Aetna representative to review your specific benefits for services like medical detox, residential rehab, outpatient programs, and therapy.
Pre-Approval Process
Many substance abuse treatment services require pre-approval from Aetna before you are admitted. This allows them to verify your medical necessity and ensure the program meets their criteria for coverage. Work closely with the treatment center to provide all required documentation for a smooth pre-authorization process.
Appealing Denials
If certain services are initially denied by Aetna, you have rights to appeal that decision. Provide additional supporting evidence from your doctor or treatment team. Clearly explain why these services are medically necessary for your recovery. Persistence may be required, but approved services could make quality care much more affordable.
Recent studies show health plans like Aetna are increasingly covering a full continuum of evidence-based addiction treatment. With some diligence navigating their requirements, you can access the comprehensive care you need to achieve lasting sobriety.
How Many Times Aetna Will Pay for Rehab
Coverage Requirements
Under the Mental Health Parity and Addiction Equity Act (MHPAEA), Aetna health insurance plans must provide the same level of coverage for addiction treatment as they do for other medical conditions. This means there are typically no limits on how many times Aetna will pay for rehab, as long as the treatment is deemed medically necessary.
Determining Medical Necessity
Aetna works directly with treatment providers like Evoke Wellness at Miramar to assess each client’s case and determine if continued rehab care meets their criteria for medical necessity. Factors they consider include the severity of the addiction, co-occurring mental health issues, past treatment history, and progress in recovery.
Covered Services
When rehab is approved, Aetna’s coverage can include a wide range of addiction treatment services with minimal out-of-pocket costs for the client. This may encompass inpatient or outpatient programs, detox, medication-assisted therapies, individual and group counseling, and other evidence-based treatment methods.
Verifying Benefits
To ensure maximum coverage, Evoke Wellness verifies each client’s specific Aetna plan details and explores all available payment options. Their goal is to provide affordable, high-quality care that supports long-term recovery from substance use disorders.
Costs of Rehab in Nashville With and Without Aetna
Tackling substance abuse often requires comprehensive treatment. With the right insurance coverage, the costs can be manageable – allowing you to prioritize your recovery journey.
Aetna Coverage Benefits
- Substance use disorder treatment programs, including detox, inpatient, and outpatient services
- Dual diagnosis treatment for co-occurring mental health conditions
- Medication-assisted treatment
- Family therapy and counseling
Out-of-Pocket Expenses
Even with Aetna insurance, you may still face some out-of-pocket costs like:
- Deductibles: The amount you pay before your plan starts covering expenses
- Copays: Fixed fees for doctor visits, prescriptions, etc.
- Coinsurance: Your percentage of costs after meeting the deductible
Potential Savings
According to a recent study, individuals with private insurance plans like Aetna can save thousands on addiction treatment compared to paying out-of-pocket. Proper coverage allows you to access quality care while managing expenses effectively.
Exploring Options
Evoke Wellness at Miramar offers personalized treatment plans tailored to your needs and Aetna benefits. Our admissions team can guide you through coverage details, out-of-pocket estimates, and financial assistance options if needed.
Prioritizing your well-being is invaluable. With the right support, achieving lasting recovery is possible – even with the initial costs involved.
FAQ: What is Aetna Insurance?
Aetna is a major health insurance provider that covers substance abuse and mental health treatment. Under the Mental Health Parity and Addictions Equity Act (MHPAEA), insurance plans must provide the same level of benefits for substance abuse treatment as they do for medical/surgical care.
Coverage at Evoke Wellness
At Evoke Wellness at Miramar, we work directly with Aetna and other insurance providers to verify each client’s coverage and design a treatment program structured so that costs are largely covered by their plan. This includes:
- Substance use disorder treatment programs
- Dual diagnosis treatment for co-occurring disorders
- Medical detox services
- Residential rehab
- Extended residential care
- Individual and group therapy
- Evidence-based therapies like acceptance and commitment therapy (ACT)
Verifying Your Benefits
Our admissions team is experienced in locating substance abuse and mental health treatment benefits within Aetna policies. We will go over your specific plan details to determine your coverage amounts and expected out-of-pocket costs.
Even if you don’t have active insurance, Evoke Wellness offers self-pay options and payment plans to make high-quality care affordable. Our goal is to minimize the financial burden so you can focus on your recovery.
Conclusion
In conclusion, navigating Aetna drug rehab coverage and treatment options can be complex, but understanding your benefits is crucial for accessing quality care.
Recent studies show that 60% of individuals with substance use disorders also have a co-occurring mental health condition, highlighting the importance of integrated treatment approaches. By utilizing evidence-based therapies like Acceptance and Commitment Therapy, you can maximize your chances of successful recovery. Remember, Aetna’s commitment to mental health parity means you have access to the care you need. Take the first step towards recovery by exploring your Aetna drug rehab options today.
Begin Your Journey with Evoke Wellness at Miramar
If you or a loved one is considering treatment, Evoke Wellness at Miramar invites you to contact us. Our compassionate team is ready to answer your questions, discuss your needs, and help you take the first steps toward recovery. In Miramar, you’ll find more than just a treatment program – you’ll discover a community dedicated to your wellness and success. Together, let’s embrace the journey to recovery and the promise of a new beginning. Call us at (833) 819-6066 today or reach out online.